Get full access with a free account
Benefits of the Coloplast® Professional Educational platform
- Get full access to all educational content, events and resources
- Track your progress
- Share content with your colleagues
- Share supporting material with your patient
Managing bowel health can be complex, especially when navigating insurance policies and reimbursement for essential supplies and treatments. This page aims to simplify that journey by offering clear insights into current coverage guidelines for bowel management tools and therapies.
For any questions, please reach out to our Reimbursement and Market Access team at USreimbursement@coloplast.com
Medicare Program Outline
Medicare is a federal insurance program that covers individuals who are 65 years of age or older, people under age 65 with certain disabilities and people of all ages with end-stage renal disease (permanent kidney failure requiring dialysis or a kidney transplant).
Medicare is an 80/20 plan, meaning Medicare covers 80% and the remaining 20% is the beneficiaries responsibility.
- For any item to be covered by Medicare, it must:
- Be eligible for a defined Medicare benefit category,
- Be reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member, and
- Meet all other applicable Medicare statutory and regulatory requirements. Information provided in this policy article relates to determinations other than those based on Social Security Act §1862(a)(1)(A) provisions (i.e. “reasonable and necessary”).
Part A - Hospital Insurance
- Hospital Stays
- SNF
- Hospice
- Some Home Health
Part B - Medical Insurance
- Outpatient care
- Physical & Occupational Therapy
- DME (medical supplies included)
- Some Home Health
Part C - Medicare Advantage
- Commercial Insurances offer Medicare Benefits
Part D - Prescription Drug Coverage
- Beneficiary pays a monthly premium
How Peristeen® Plus works
Water is introduced into the rectum and colon via the anus and subsequently evacuated into a toilet together with the contents of the descending colon, sigmoid and rectum.
Who can use Peristeen® Plus
Peristeen® Plus is an FDA approved device indicated for use by children (2 years -<12 years), adolescents (12 years - < 18 years transitional adolescents (18 years - <21 years) and adult patients with neurogenic bowel dysfunction (NBD) who suffer from fecal incontinence, chronic constipation and/or time-consuming bowel management procedures.
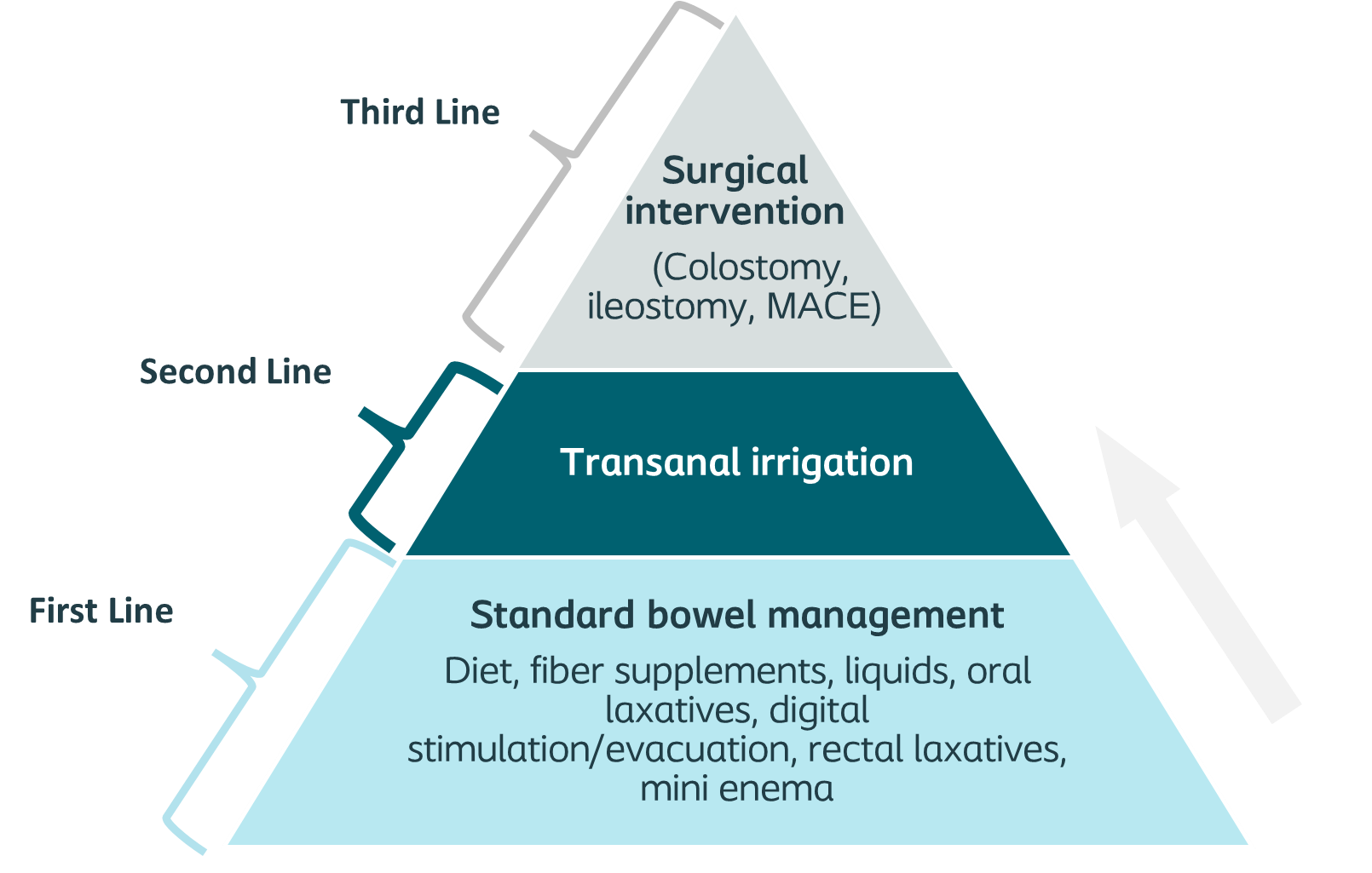
TAI is considered when first line treatments fail to provide sufficient relief from symptoms of fecal incontinence or constipation
A stepwise approach to treating neurogenic bowel dysfunction, building from more conservative first-line interventions to second-line treatments like Peristeen and finally to invasive surgical treatments, including stoma surgery.
Medicare covers Peristeen® Plus as of April 1, 2025
The Centers for Medicaid and Medicare Services (CMS) issued a positive final Benefit Category Determination (BCD)1 for transanal irrigation (TAI) devices and accessories. Effective April 1, 2025, devices with rectal catheters with a sealing function (e.g., balloon or cone-based catheters) are considered “prosthetic devices.” In addition, the Bowel Management Devices Local Coverage Determination (LCD) L362672 was updated to remove previous non-coverage language for manual pump systems.
The Bowel Management Devices-Policy Article (A54516)3 outlines coding and billing guidelines for Peristeen Plus. For Medicare beneficiaries, individual coverage of Peristeen Plus is based on medical necessity. Documentation in the medical record must reflect the medical need for transanal irrigation.
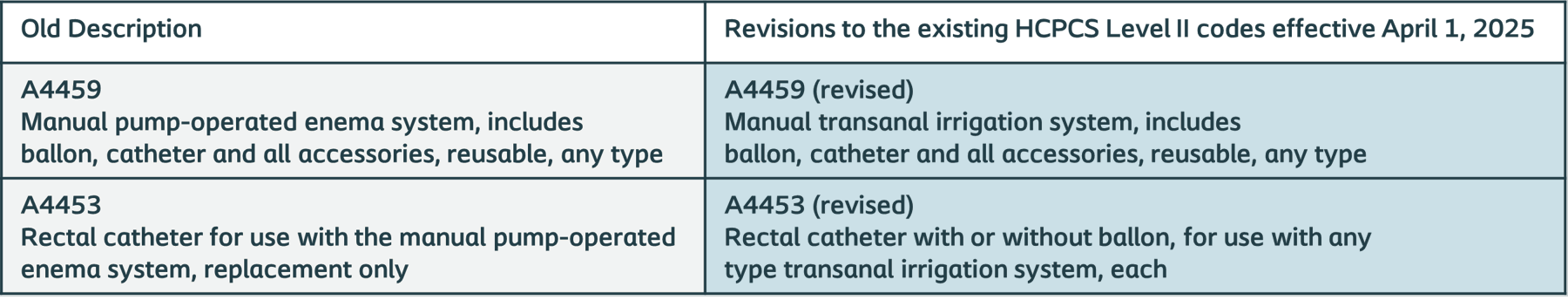
Revisions1 to the existing HCPCS Level II codes, effective April 1, 2025, as well as final Medicare reimbursement,4 effective October 1, 2025, are below.
Learn more: Peristeen Plus Medicare Update
Understanding Medicare Reimbursement and Coverage:
Medicare Coverage: Peristeen Plus is covered under Medicare Part B.
Medicare Deductible: Medicare beneficiaries have a yearly deductible that must be met before Medicare pays any claims.4
Medicare Out of Pocket Costs: After the deductible is met, Medicare beneficiaries have a 20% coinsurance responsibility. 4 Beneficiaries with supplemental insurance may incur less out of pocket cost. DME providers may be able to provide a patient out of pocket cost estimate.
Medicare Advantage Coverage: Medicare Advantage plans must cover all medically necessary services that Original Medicare covers.5
Medicare Advantage Deductible: Medicare Advantage beneficiaries may have a yearly deductible that must be met before the Medicare Advantage plan pays any claims.
Medicare Advantage Out of Pocket Costs: Reimbursement and beneficiary out of pocket costs varies and is dependent on the supplier’s contract with the Medicare Advantage health plan. DME providers may be able to provide a patient out of pocket cost estimate.
Prepare your Clinic Coloplast is available to clinically train your team on transanal irrigation with Peristeen Plus today! Contact your local Territory Manager to schedule a training.
Medicaid Information Overview
Each state Medicaid program maintains its own fee schedule for Durable Medical Equipment (DME), which outlines the reimbursement rates for items like transanal irrigation system (TAI). These fee schedules vary widely by state and are updated periodically to reflect changes in policy, pricing, and medical necessity
Rather than administering all benefits directly, most states contract with Managed Care Organizations (MCOs) to deliver Medicaid services, including DME. This model is known as Managed Medicaid.
Managed Medicaid plans are private health plans that operate under contract with state Medicaid agencies. These contracts require MCOs to:
- Build provider networks
- Handle prior authorizations and utilization management
- Coordinate care for enrollees
- Ensure access to covered services, including DME
States individually contract with these plans, often through competitive procurement processes. These contracts are reviewed by the Centers for Medicare & Medicaid Services (CMS) to ensure compliance with federal regulations
Managed Medicaid coverage and reimbursement
- Follows Medicaid coverage and can provide additional benefits
- Reimbursement can be different than Medicaid
- Managed Medicaid plan contract with suppliers at rates typically discounted from Medicaid fee schedule
- DME Suppliers need to contract with each plan
Commercial coverage and reimbursement
- Broad commercial coverage with national and regional payors
